Sleep quality
How does sleep quality relate to cognitive and brain integrity?
By Géraldine Rauchs
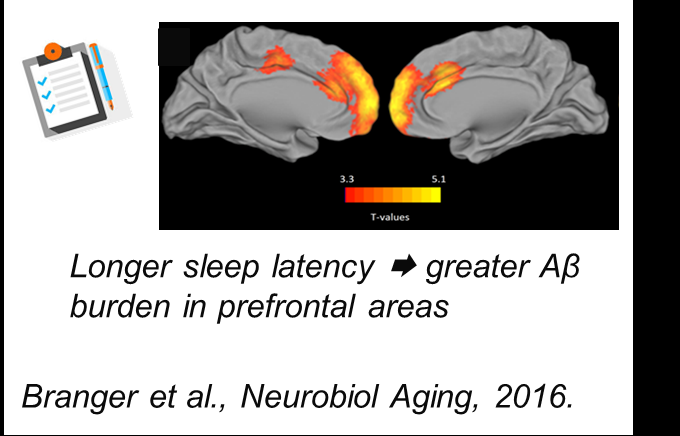
In the Silver Santé Study, my group investigates how sleep quality, assessed using different tools (questionnaires, actigraphy and polysomnography), is associated with cognitive and brain alterations in older adults. Indeed, sleep quality may represent a modifiable risk factor for cognitive decline and dementia. However, sleep disturbances may also be an early manifestation of Alzheimer’s disease, associated with reduced quality of life and due to the degeneration of some brain areas involved in sleep. We have started this project with Gaël Chételat a few years ago with the IMAP+ cohort. We first showed that cognitively normal older individuals who complain of recurring difficulties falling asleep have greater amyloid deposition, lesions typical of Alzheimer’s disease, in the prefrontal cortex, known to be early altered in this disease (Branger et al., 2016; Fig. 1). In addition, people who suffer from multiple awakenings during the night have also lower grey matter volume in the insula, a region important for some sleep rhythms. Then, we further explored the links between sleep fragmentation, brain and cognition using wrist actigraphy. This device allows to assess the activity-rest cycle of participants in their usual environment. Greater sleep fragmentation is associated with lower executive functioning and functional and molecular brain changes especially in the frontal cortex, the hippocampus and the thalamus. However, these links were observed only in cognitively normal individuals, and not in patients with subjective or objective cognitive decline (André et al., 2019), suggesting that treating sleep disturbances before the onset of cognitive signs may help to cope with brain alterations and maintain an efficient cognitive functioning.
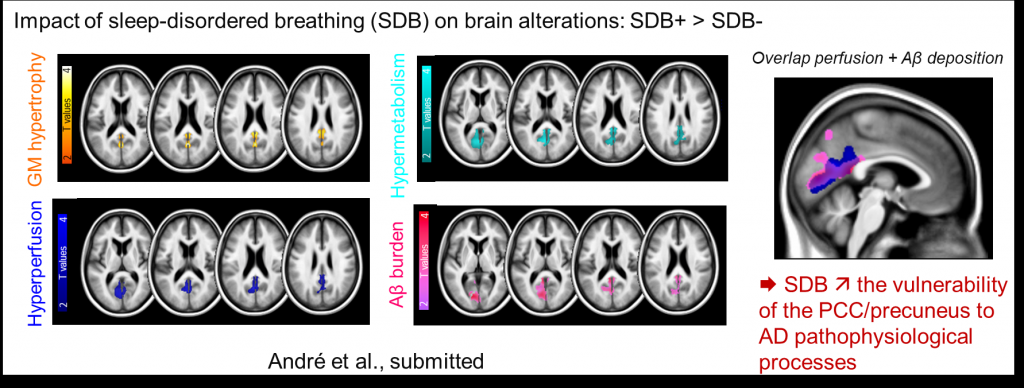
Finally, using baseline data from the AGEWELL randomized controlled trial of the Silver Santé Study H2020 European project, we investigated the impact of sleep apnea on the brain. We found that cognitively healthy elders showing a significant number of apneas per hour of sleep had brain changes, including more grey matter, more glucose and oxygen consumption, and more amyloid deposition. These brain changes overlapped in the posterior cingulate cortex and the precuneus, brain areas particularly vulnerable to Alzheimer’s disease (André et al., 2010; Fig. 2). Moreover, they occur covertly, without any signs of cognitive deficits, self-reported cognitive or sleep difficulties, or excessive daytime sleepiness (which is one of the symptoms of sleep apnea). The combination of multiple neuroimaging techniques also allowed us to precise the potential mechanisms underlying these links, notably inflammatory processes. These results support the need to screen and treat for sleep apnea in older adults to reduce Alzheimer’s disease risk.
In brief, all these studies suggest that to age well, you must sleep well. Over and above, they provide first evidence to identify the mechanisms underlying the relationships between sleep difficulties and AD risk.
Links to publications :
- Branger et al. (2016) : https://doi.org/10.1016/j.neurobiolaging.2016.02.009.
- André et al. (2019) : https://doi.org/10.1016/j.dadm.2018.12.009.
- André et al. (2020) : https://doi.org/10.1001/jamaneurol.2020.0311.
Current PhD students :
Pierre Champetier
Valentin Ourry
Alumnis :
Claire André, PhD
Pierre Branger, MD
Stéphane Rehel, PhD